Rethinking Metabolism, Aging, and Energy from the Cellular Core
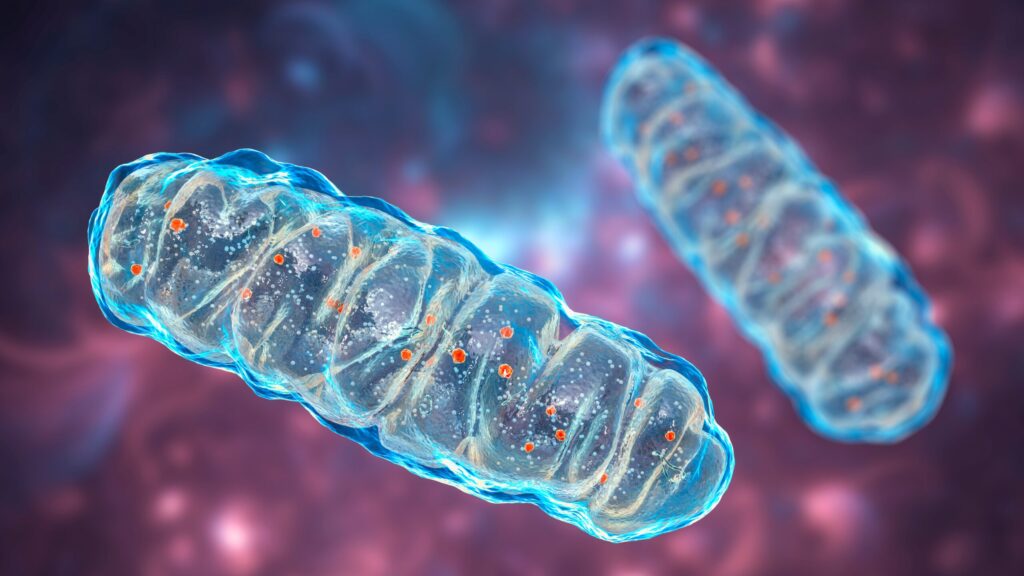
When we think of type 2 diabetes, the first culprits that come to mind are often sugar, insulin, or perhaps lifestyle choices like diet and exercise. But scientists are increasingly turning their attention inward—deep into the cell—to uncover a less obvious but fundamental player: the mitochondria.
Often called the “powerhouses” of the cell, mitochondria do far more than just produce energy. They help regulate metabolism, cellular stress responses, and even the way our genes are expressed. And when they begin to falter, the effects can be systemic and severe.
A recent study published in Nature Metabolism explores this intricate relationship, offering compelling evidence that mitochondrial dysfunction isn’t just a symptom of metabolic disease—it may be a key driver. The implications stretch far beyond diabetes, touching on aging, inflammation, and cellular resilience.
Let’s explore how these microscopic engines work, how they break down, and what this new understanding could mean for preventing and treating metabolic disorders.
A Quick Primer: What Are Mitochondria?
Every cell in your body—except red blood cells—contains hundreds to thousands of mitochondria. These tiny organelles are responsible for generating ATP (adenosine triphosphate), the molecule your body uses as its primary energy currency.
But their role goes far beyond fueling muscles or neurons. Mitochondria also:
- Help regulate calcium balance
- Modulate immune responses
- Play a key role in apoptosis (programmed cell death)
- Generate reactive oxygen species (ROS) as byproducts of respiration
- Influence inflammation and hormonal signaling
Because of this complexity, mitochondrial health is considered a foundational pillar of both metabolic health and aging biology.
The Link Between Mitochondria and Type 2 Diabetes
Type 2 diabetes is marked by a resistance to insulin, the hormone that helps cells absorb glucose from the bloodstream. Over time, insulin resistance leads to elevated blood sugar, inflammation, and damage to organs.
But what causes insulin resistance in the first place?
Historically, the blame has been placed on:
- Obesity and fat accumulation
- Sedentary lifestyle
- Genetic predisposition
However, mounting evidence suggests that mitochondrial dysfunction is a hidden—but central—trigger. When mitochondria can’t effectively process nutrients, particularly fatty acids and glucose, cells begin to mismanage energy, leading to metabolic chaos.
The Study: Connecting Mitochondrial DNA Damage and Diabetes
In this latest investigation, researchers studied both mice and human tissue samples to explore how mitochondrial health correlates with insulin sensitivity. They focused specifically on mitochondrial DNA (mtDNA)—the small, circular genome found inside mitochondria, separate from the DNA in the cell’s nucleus.
What they found was striking:
- Mice with elevated mtDNA damage showed clear signs of insulin resistance and glucose intolerance.
- Damaged mtDNA appeared to activate inflammatory pathways, particularly through sensors like cGAS and STING—proteins that detect DNA in the wrong place (such as outside the mitochondria) and interpret it as a sign of infection.
- This triggered a cascade of inflammation, including the activation of interferons and other immune signals.
In essence, when mitochondria shed damaged DNA, the immune system interprets it as a threat—leading to a chronic, misdirected inflammatory state that undermines insulin signaling.
Inflammation: The Silent Amplifier
This insight helps explain why type 2 diabetes is not just a problem of blood sugar, but a condition deeply intertwined with chronic, low-grade inflammation—sometimes called “metaflammation.”
Mitochondrial damage, it turns out, may be the spark that ignites this process. Once the cGAS-STING pathway is triggered by leaking mtDNA, it kicks off a self-reinforcing cycle:
- Inflammation increases oxidative stress
- Oxidative stress damages more mitochondria
- More mtDNA leaks out, triggering further inflammation
This vicious loop not only impairs insulin sensitivity but may also accelerate aging and damage to tissues like the liver, pancreas, and blood vessels.
The Muscle Connection: Why Skeletal Muscle Matters
Skeletal muscle is the body’s largest organ by mass and a major site of glucose uptake. It’s also rich in mitochondria—needed to power everything from walking to weightlifting.
In people with type 2 diabetes, skeletal muscle often shows signs of mitochondrial decline, including:
- Decreased mitochondrial content
- Impaired respiration
- Accumulation of lipid byproducts (which interfere with insulin signaling)
The study highlighted that in muscle cells specifically, mitochondrial DNA damage led directly to impaired insulin action, reinforcing the idea that muscle is both a target and a contributor in diabetes pathophysiology.
Why This Matters: Aging, Longevity, and Energy Resilience
This research doesn’t just clarify the biology of diabetes—it deepens our understanding of aging itself.
As we grow older, mitochondrial quality tends to decline, leading to a drop in cellular energy, increased oxidative stress, and systemic inflammation—factors central to many age-related diseases, including:
- Type 2 diabetes
- Cardiovascular disease
- Alzheimer’s and neurodegeneration
- Sarcopenia (muscle loss)
The shared thread? Mitochondrial dysfunction.
By viewing diabetes through this lens, we begin to see it not as a standalone disease, but as a manifestation of deeper biological aging. This opens the door to novel therapies that don’t just treat symptoms—but support cellular resilience and bioenergetic health.
Therapeutic Possibilities: What Can Be Done?
Armed with these insights, scientists and biotech companies are exploring multiple ways to target mitochondrial health in the fight against metabolic disorders.
1. Mitochondria-Protective Compounds
- Urolithin A: A compound found in pomegranate that supports mitophagy (the clearance of damaged mitochondria).
- Nicotinamide riboside (NR) and NMN: NAD+ precursors that support mitochondrial energy production.
- MitoQ and SkQ1: Mitochondria-targeted antioxidants designed to reduce oxidative damage.
2. Modulating the cGAS-STING Pathway
Some pharmaceutical candidates are aimed at blocking the immune overreaction triggered by mtDNA, dampening inflammation without suppressing healthy immune function.
This could help break the cycle of mitochondrial damage and chronic inflammation.
3. Exercise and Lifestyle Interventions
No surprise here: exercise remains one of the most powerful boosters of mitochondrial function. It stimulates:
- Mitochondrial biogenesis (making more mitochondria)
- Improved insulin sensitivity
- Reduced mtDNA damage
Even modest activity, like brisk walking or resistance training, can have meaningful effects—especially when paired with a nutrient-dense, anti-inflammatory diet.
What This Means for You: A Practical, Holistic Approach
If you’re concerned about blood sugar, insulin resistance, or simply want to age with more vitality, consider these strategies to support mitochondrial health:
Eat to Energize
- Prioritize whole, minimally processed foods
- Include polyphenol-rich produce (e.g., berries, leafy greens)
- Embrace healthy fats from sources like olive oil, nuts, and fish
- Reduce intake of refined sugar and seed oils
Move With Intention
- Engage in regular aerobic activity (30 minutes/day)
- Include strength training to stimulate muscle mitochondria
- Don’t underestimate the value of walking, stretching, or even dancing
Rest and Repair
- Sleep deeply and consistently—mitochondria regenerate during sleep
- Manage stress through breathing exercises, meditation, or journaling
- Avoid smoking, excess alcohol, and chronic exposure to pollutants
Consider Targeted Support (With Guidance)
- Talk to a longevity-informed healthcare provider about NAD+ boosters or mitophagy-promoting supplements
- Track your metabolic health with tests like fasting insulin, HOMA-IR, or continuous glucose monitors
Final Thoughts: The Future of Metabolic Health Starts at the Cellular Level
The new understanding of type 2 diabetes as a mitochondrial disease is more than just a shift in scientific framing. It’s a call to reimagine how we prevent and treat chronic illness—not by managing numbers on a chart, but by restoring the body’s innate capacity for energy, resilience, and self-repair.
Mitochondria may be tiny, but they hold a disproportionate influence on how we age, how we feel, and how we function.
By protecting and nourishing these cellular engines, we don’t just support metabolic health—we support a longer, more vibrant life.
