For millions worldwide, osteoarthritis represents one of the most common—and painful—conditions of aging. While often dismissed as an inevitable consequence of wear and tear, scientists are uncovering that osteoarthritis, particularly in women, may be influenced not just by mechanical stress, but by something far more subtle: hormonal balance.
New research examining the roles of estradiol and progesterone, two essential sex hormones, sheds light on how these hormones may shape the progression of knee osteoarthritis (KOA)—the most prevalent form of arthritis that affects mobility, independence, and quality of life as we age.
The findings offer promising insights, especially for postmenopausal women, into how hormonal shifts may not only contribute to joint degeneration but also open the door to potential protective strategies.
The Gendered Face of Osteoarthritis
Osteoarthritis affects both men and women, but after age 50, women experience a steep rise in incidence. By age 65, nearly 70% of women show radiographic signs of knee osteoarthritis.
Why the discrepancy?
Many scientists point to hormonal changes—particularly the sharp drop in estradiol (a primary form of estrogen) and progesterone—during menopause. These hormones are known to influence:
- Bone density
- Muscle mass
- Inflammatory signaling
- Cartilage health
- Joint lubrication
This suggests that osteoarthritis may not simply be a wear-and-tear condition, but rather a complex interplay between mechanical stress, hormonal fluctuations, and systemic inflammation.
Estradiol: More Than a Reproductive Hormone
Estradiol is widely recognized for its role in regulating female reproductive cycles. But beyond fertility, estradiol supports a host of metabolic and musculoskeletal functions that become increasingly important with age.
In Joint Health, Estradiol May:
- Inhibit inflammatory cytokines that drive cartilage breakdown
- Promote collagen synthesis in cartilage
- Improve joint lubrication via synovial fluid
- Support subchondral bone strength (the bone just beneath cartilage)
As estradiol levels decline during menopause, these protective effects wane, leaving joints more vulnerable to damage, inflammation, and degeneration.
Progesterone’s Underappreciated Role
While progesterone is often viewed through the lens of reproduction, emerging research suggests it also plays a role in modulating joint health.
Progesterone may:
- Exert anti-inflammatory effects
- Support tissue remodeling and repair
- Regulate immune cell activity within joint spaces
Its decline, alongside estradiol, may amplify the inflammatory and catabolic processes that drive cartilage loss and pain in osteoarthritis.
The Study: Evaluating Hormonal Influence on Knee Osteoarthritis Progression
In the recent study titled “Effects of Estradiol and Progesterone on Knee Osteoarthritis”, researchers examined data from a cohort of postmenopausal women diagnosed with knee osteoarthritis. The study’s goal was simple but profound: to explore whether varying levels of estradiol and progesterone correlated with differences in the severity or progression of knee osteoarthritis.
Key Study Highlights:
- Participants: Postmenopausal women with confirmed knee osteoarthritis
- Hormone levels measured: Blood serum levels of estradiol and progesterone
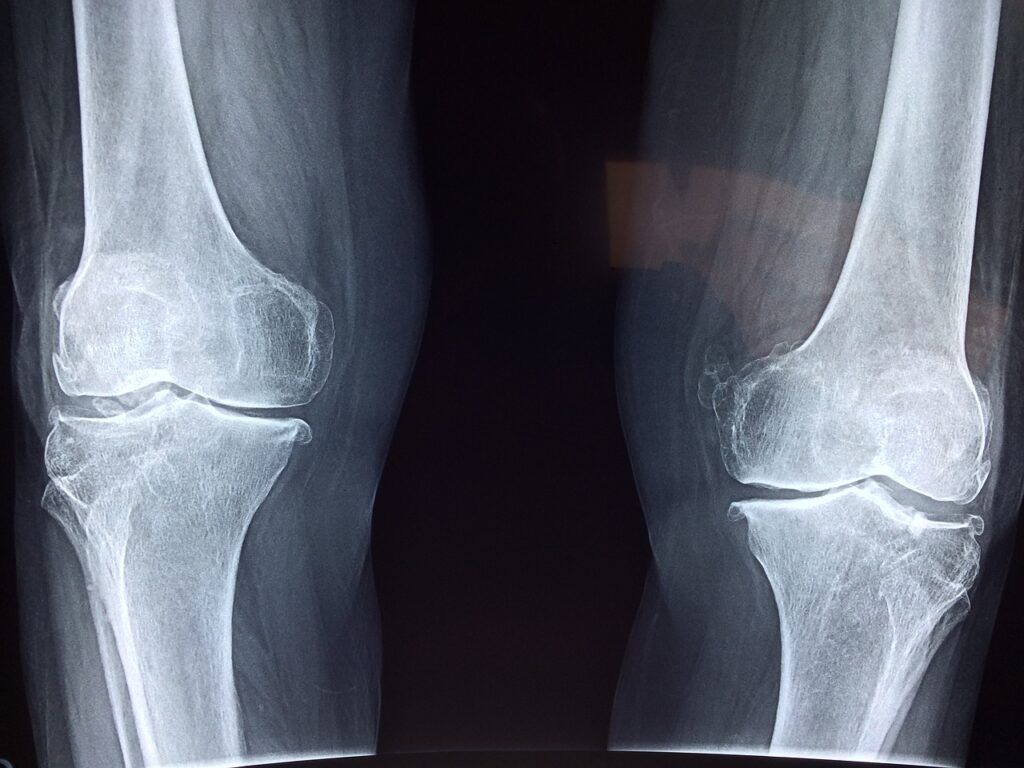
- Osteoarthritis severity assessed through radiographic imaging and symptom scoring (pain, stiffness, and function)
By analyzing this relationship, the researchers hoped to clarify whether hormone levels might be contributing factors to disease progression—or even serve as potential targets for future interventions.
Findings: Protective Trends, But Not Causation
The study’s results offer encouraging but nuanced conclusions.
- Women with higher estradiol levels showed a modest reduction in osteoarthritis severity.
- Similarly, higher progesterone levels were associated with less joint degeneration and better physical function.
- However, when controlling for other factors (like body mass index, physical activity, or inflammation markers), these associations weakened and did not reach strong statistical significance.
In other words, while elevated hormone levels may trend toward protective effects, the relationship is likely complex and influenced by multiple overlapping biological processes.
The study’s authors emphasize that larger, long-term trials are needed to confirm these findings and fully untangle the hormonal contributions to osteoarthritis risk.
Inflammation: The Common Thread
One of the most intriguing aspects of both estradiol and progesterone is their ability to modulate inflammation—a central player in osteoarthritis progression.
When estrogen levels drop:
- Pro-inflammatory cytokines such as IL-1β, IL-6, and TNF-α rise.
- This fuels cartilage breakdown and synovial inflammation.
- The joint becomes more vulnerable to structural degradation.
Progesterone also influences inflammatory pathways, though its mechanisms remain less thoroughly studied. Some research suggests it can inhibit nitric oxide synthesis and matrix metalloproteinases—two compounds involved in cartilage destruction.
Together, these hormonal shifts may create an inflammatory environment that accelerates joint damage during midlife and beyond.
Weight, Hormones, and Osteoarthritis: An Interwoven Triad
An important caveat in hormone research is the significant overlap between body weight, metabolic health, and joint disease.
- Higher body mass index (BMI) not only adds mechanical load to the knee but also increases systemic inflammation.
- Adipose (fat) tissue is hormonally active, producing both estrogen and pro-inflammatory compounds.
- This creates a complex feedback loop where hormonal changes, weight gain, and inflammation may collectively worsen osteoarthritis risk.
For this reason, weight management remains one of the most effective non-pharmaceutical strategies to slow osteoarthritis progression—independent of hormone levels.
Could Hormone Therapy Help?
Given estradiol and progesterone’s potential protective roles, many wonder: could hormone replacement therapy (HRT) slow osteoarthritis progression?
The evidence here is mixed.
- Some observational studies suggest that HRT may reduce joint pain and stiffness in postmenopausal women.
- However, randomized controlled trials have yielded inconsistent results.
- Current guidelines do not recommend HRT specifically for osteoarthritis, though it may offer ancillary joint benefits when prescribed for other menopausal symptoms.
Ultimately, any consideration of HRT must carefully weigh individual risks and benefits, particularly concerning cardiovascular health, breast cancer risk, and bone density.
Other Emerging Therapies Targeting Inflammation and Cartilage
While hormones may play a role, multiple other pathways are being explored to support joint health and potentially slow or reverse osteoarthritis progression:
- Senolytics: Drugs that selectively remove senescent cells implicated in joint inflammation.
- Regenerative therapies: Platelet-rich plasma (PRP), stem cell injections, and exosomes to support cartilage repair.
- Mitochondrial support: Nutrients like Urolithin A that may promote cellular cleanup (mitophagy) and energy metabolism in joint tissues.
- Nutraceuticals: Collagen peptides, curcumin, and omega-3s have shown mild benefits for joint pain and function.
While these approaches are still evolving, they reflect an exciting shift in osteoarthritis research: a move away from simply masking pain toward addressing the underlying biology of joint aging.
What You Can Do Now to Protect Joint Health
While many pharmaceutical interventions remain in development, lifestyle choices remain our most accessible and reliable tools for preserving joint function as we age:
1. Prioritize Weight Management
Every extra pound adds significant stress to the knees. Modest weight loss can reduce joint load and inflammation.
2. Stay Physically Active
Low-impact activities like swimming, cycling, yoga, and strength training help maintain cartilage health and strengthen surrounding muscles for joint support.
3. Eat an Anti-Inflammatory Diet
- Emphasize whole foods: vegetables, fruits, legumes, fatty fish, and healthy fats like olive oil.
- Minimize processed foods and excess sugar.
4. Support Hormonal Balance
- Discuss perimenopause and menopause management with your healthcare provider.
- Explore lifestyle strategies (sleep, stress management, nutrition) that support healthy hormone function.
5. Consider Joint Supplements
Collagen peptides, curcumin, and certain antioxidant formulas may offer modest symptom relief for some individuals.
Looking Ahead: The Future of Hormones and Joint Aging
The evolving understanding of how estradiol and progesterone influence osteoarthritis offers new hope—but also reinforces the complexity of aging biology.
Rather than seeking a single “magic bullet,” researchers now recognize that joint health is shaped by a dynamic interplay between:
- Hormones
- Inflammation
- Metabolism
- Mechanical forces
- Cellular repair pathways
As longevity science advances, personalized strategies that combine targeted hormonal support with lifestyle interventions may eventually offer more effective ways to preserve joint function deep into later life.
Final Reflections
Osteoarthritis need not be seen as an inevitable consequence of getting older. This study adds to a growing body of research revealing that hormones like estradiol and progesterone are not simply reproductive players—they are guardians of broader musculoskeletal health.
While further research is needed, one thing remains clear: how we move, eat, and care for our bodies in midlife has profound ripple effects for how we experience mobility, independence, and vitality as the years advance.
The takeaway is hopeful: by honoring our biology today, we can better protect our freedom of movement tomorrow.
