As longevity science moves beyond simply managing chronic disease and into restoring function at the cellular level, one emerging field stands out: exosome therapy. These microscopic messengers may soon reshape how we approach some of the most challenging aspects of aging — particularly when it comes to preserving and rejuvenating heart health.
A growing body of research is revealing how exosomes, tiny vesicles secreted by cells, can orchestrate powerful regenerative processes throughout the body. In particular, their role in cardiac repair offers hope for millions of people facing age-related cardiovascular decline — one of the leading causes of death and disability worldwide.
Let’s explore what exosomes are, how they impact heart health, and why they may play a critical role in the future of longevity medicine.
The Aging Heart: Why Cardiac Health Is Central to Longevity
Cardiovascular disease remains the number one cause of death globally, responsible for nearly one-third of all deaths each year. As we age, our hearts become more vulnerable to:
- Stiffening of arteries (arteriosclerosis)
- Loss of elasticity in heart muscle tissue
- Impaired energy production in cardiac cells
- Reduced vascular repair capabilities
- Chronic low-grade inflammation that erodes vascular function
Even in individuals without overt heart disease, these cumulative changes contribute to decreased stamina, poor circulation, and increased frailty in later life.
While traditional approaches — like blood pressure management, cholesterol control, and medications — can slow progression, they typically do little to restore damaged cardiac tissue once it has deteriorated.
This is where regenerative approaches like exosome therapy may offer transformative possibilities.
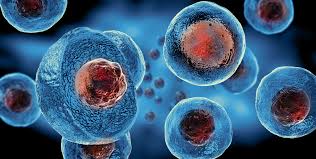
What Are Exosomes?
Exosomes are nano-sized extracellular vesicles, typically measuring 30–150 nanometers in diameter. Every cell in the body releases exosomes into the bloodstream as part of its normal communication system.
Inside these tiny vesicles are powerful molecular messengers, including:
- Proteins
- Lipids
- Messenger RNA (mRNA)
- MicroRNA (miRNA)
- Growth factors
Exosomes function like biological “text messages” that allow cells to coordinate complex repair, immune, and metabolic responses without direct contact. They have been described as the body’s natural information carriers, influencing everything from wound healing to stem cell activation.
Exosomes and Cardiac Repair: The New Data
Recent studies have shown that exosomes may play a vital role in protecting and even regenerating heart tissue — particularly after injury such as:
- Myocardial infarction (heart attack)
- Ischemia-reperfusion injury (oxygen deprivation)
- Chronic cardiac fibrosis (scarring of the heart muscle)
- Age-related decline in cardiac stem cell activity
In preclinical models, administration of exosomes derived from stem cells — especially mesenchymal stem cells (MSCs) — has led to:
- Reduced inflammation in damaged heart tissue
- Promotion of new blood vessel formation (angiogenesis)
- Decreased fibrosis and scarring
- Improved cardiac output and contractile function
Unlike direct stem cell injections, which present challenges of safety, rejection, or abnormal growth, exosomes deliver cell-free regenerative signals without introducing whole cells — potentially reducing the risk profile significantly.
Why Exosomes May Be Safer Than Stem Cells
While stem cell therapies have long generated excitement, they carry certain inherent risks:
- Potential for tumor formation (teratomas)
- Difficulty in controlling where transplanted cells migrate
- Immune rejection in some cases
Exosomes sidestep many of these issues by delivering the same beneficial signals stem cells produce, but without the cells themselves. This allows for more targeted, controlled therapeutic use while minimizing side effects.
For cardiac repair, this cell-free approach may ultimately prove both safer and more scalable.
The Anti-Inflammatory Power of Exosomes
One of the most promising aspects of exosome therapy for heart health lies in its ability to modulate chronic inflammation.
As we age, low-level inflammation (often referred to as inflammaging) damages blood vessels, weakens heart muscle, and contributes to the development of:
- Atherosclerosis
- Hypertension
- Heart failure
- Arrhythmias
Exosomes derived from MSCs have been shown to downregulate pro-inflammatory cytokines while boosting anti-inflammatory signals. This helps:
- Protect endothelial cells lining blood vessels
- Prevent arterial stiffening
- Improve vascular flexibility
- Support healthy oxygen and nutrient delivery to tissues
Exosomes and Mitochondrial Health: The Energy Connection
Another fascinating avenue of research is how exosomes may support mitochondrial function, which declines sharply in aging heart cells.
Mitochondria are responsible for generating ATP — the energy currency of cells. As they fail, the heart struggles to meet its high energy demands.
Exosome treatments may:
- Deliver mitochondrial RNA and proteins that restore energy production
- Reduce oxidative stress by improving mitochondrial resilience
- Enhance mitophagy (the cleanup of damaged mitochondria)
- Normalize calcium handling, which regulates cardiac muscle contraction
This mitochondrial support may make exosomes a powerful tool not just for those recovering from cardiac events, but also for preventing age-related cardiovascular decline in healthy individuals.
Clinical Trials: Moving from Lab to Clinic
While much of the excitement around exosomes has been generated in laboratory models, human clinical trials are beginning to emerge.
Early phase studies have explored exosome therapy in:
- Post-myocardial infarction recovery
- Heart failure management
- Cardiomyopathy and heart muscle inflammation
- Diabetic vascular complications
Though still in their infancy, initial results have shown promising safety profiles, with some patients experiencing improvements in cardiac output, exercise tolerance, and quality of life.
Larger-scale, randomized controlled trials will be needed to confirm long-term efficacy and identify optimal dosing strategies.
Beyond the Heart: Systemic Anti-Aging Potential
One reason exosomes are attracting so much attention in the longevity community is that their benefits may extend well beyond the heart. Because they operate systemically, exosomes may support:
- Brain health (neuroinflammation reduction)
- Joint repair (cartilage regeneration)
- Skin rejuvenation (collagen and elasticity support)
- Immune modulation (autoimmune and allergy balance)
- Metabolic function (insulin sensitivity improvements)
For this reason, many researchers believe that exosome therapies may emerge as a multi-system longevity tool capable of addressing multiple aging pathways simultaneously.
Practical Considerations: Where We Are Today
While exosome science is deeply exciting, it’s important to acknowledge that much of this field remains experimental:
- Exosome production methods are still being standardized.
- Quality control and purity remain major regulatory hurdles.
- Long-term safety studies are ongoing.
- Clinical availability is currently limited to select research protocols or highly specialized clinics.
For now, exosome therapy should be viewed as an emerging, highly promising frontier — not yet ready for widespread clinical use, but moving rapidly toward broader application.
Lifestyle Foundations Still Matter
Even as regenerative therapies evolve, foundational lifestyle habits remain the cornerstone of heart health and healthy aging:
- Nutrition: Plant-forward, anti-inflammatory diets rich in polyphenols, omega-3s, and micronutrients.
- Physical activity: Both cardiovascular and resistance training to strengthen the heart and vascular system.
- Stress management: Lowering cortisol and sympathetic overactivation to protect endothelial function.
- Sleep optimization: Supporting circadian repair cycles that regulate inflammation and mitochondrial function.
- Avoidance of smoking and excess alcohol, both of which accelerate cardiovascular aging.
In time, exosome therapy may complement these strategies as an adjunctive rejuvenation tool, not a replacement for self-care.
The Future of Cardiac Longevity
The vision taking shape at the frontier of exosome research is both inspiring and realistic:
- Early interventions to preserve vascular flexibility
- Regeneration of cardiac tissue after injury
- Reduction of chronic low-grade inflammation
- Support for mitochondrial energy production deep into later life
Ultimately, exosome-based therapies may help turn back the biological clock on cardiovascular aging, extending not only lifespan but — perhaps more importantly — healthspan.
As one leading researcher recently put it:
“We may never stop the heart from aging entirely — but we may be able to help it age much more gracefully.”
Final Reflections: Hope at the Cellular Level
Exosomes represent a paradigm shift in regenerative medicine. Rather than replacing damaged cells, they aim to reactivate the body’s innate capacity for repair — a deeply elegant solution that aligns with the body’s own design.
While we’re still at the early stages of fully harnessing their potential, exosome science offers a powerful glimpse into how the next generation of longevity interventions will operate: at the molecular, cellular, and information-processing levels that truly define how we age.
As research progresses, the promise of healthier, longer lives supported by exosome-based therapies is no longer a distant dream, but an emerging reality being shaped today in labs, clinics, and longevity conferences worldwide.
