How targeting these specialized immune cells may offer novel ways to slow aging and extend healthspan
In the intricate and rapidly evolving world of aging research, cellular senescence has emerged as one of the most intriguing — and most complex — hallmarks of aging. The idea that our own cells may gradually turn into dysfunctional “zombies,” driving chronic inflammation and tissue damage, is now widely accepted as a central contributor to many age-related diseases.
Yet, as our understanding of senescence continues to deepen, researchers are uncovering that not all senescent cells are created equal. In particular, one unique class of senescent cells — senescent macrophages — may offer an especially promising target for interventions aimed at improving healthspan and delaying the degenerative effects of aging.
Let’s take a closer look at what makes senescent macrophages distinct, why they’re emerging as a critical player in the aging process, and how targeting them may unlock powerful new strategies for extending healthy human lifespan.
Macrophages: The Immune System’s Versatile Workhorses
Macrophages are part of our innate immune system, functioning as both defenders and caretakers of the body. The word “macrophage” literally means “big eater,” which perfectly describes their role: they patrol tissues and bloodstream, engulfing pathogens, clearing debris, and cleaning up dead or damaged cells.
Beyond this first-responder role, macrophages also:
- Regulate inflammation
- Help coordinate tissue repair
- Maintain homeostasis in organs like the liver, lungs, heart, and brain
- Orchestrate immune signaling between different immune cell types
In youth, macrophages work efficiently to eliminate cellular threats while supporting the body’s repair processes. However, as we age, the function and behavior of macrophages begins to change — often in ways that contribute to chronic, low-grade inflammation, or what researchers now call inflammaging.
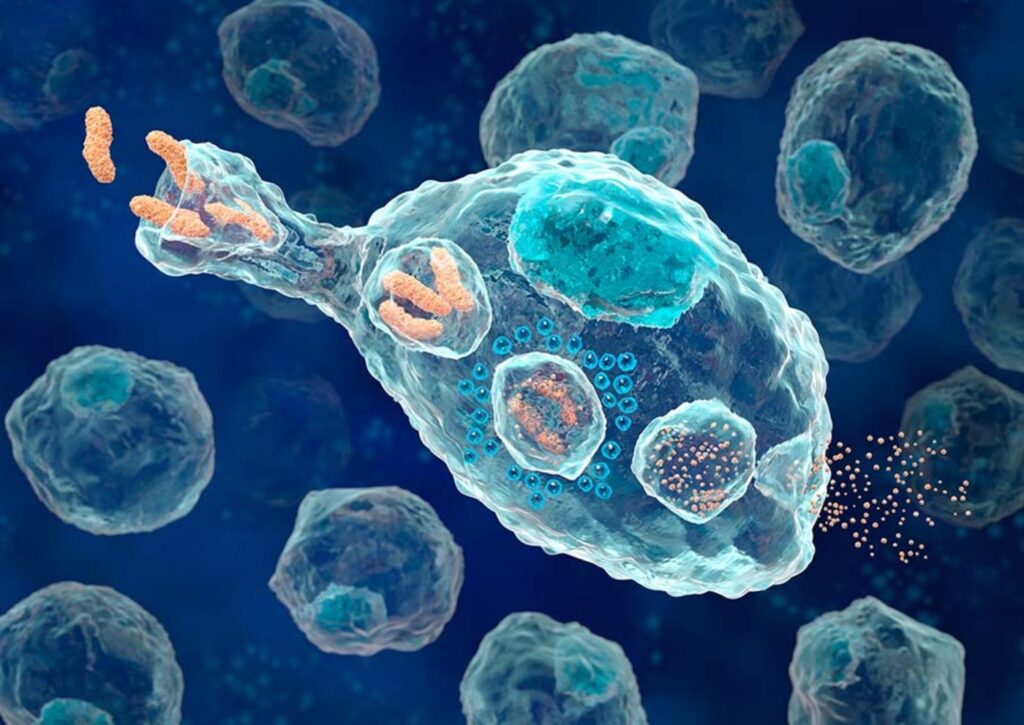
Cellular Senescence: When Macrophages Stop Performing Their Duties
Cellular senescence occurs when a cell becomes irreversibly damaged or stressed and stops dividing. These cells don’t die, but instead enter a kind of dysfunctional “survival mode,” secreting inflammatory factors that can harm neighboring cells and tissue structures.
Senescent macrophages are particularly problematic because:
- They remain metabolically active but fail to clear debris and pathogens efficiently.
- They secrete a damaging mix of senescence-associated secretory phenotype (SASP) factors — including pro-inflammatory cytokines, chemokines, and proteases.
- They contribute to the chronic activation of the immune system, perpetuating tissue damage and aging.
Over time, the accumulation of these senescent immune cells creates a pro-inflammatory feedback loop that accelerates many age-related disorders.
Why Macrophage Senescence Is a Unique Problem
Most discussions of cellular senescence focus on fibroblasts, endothelial cells, or epithelial cells. However, senescent macrophages deserve special attention because of their central role in managing inflammation and orchestrating repair across multiple tissues.
In aging individuals, senescent macrophages accumulate in multiple organs:
- Liver: Contributing to non-alcoholic fatty liver disease (NAFLD) and fibrosis.
- Heart: Promoting atherosclerosis and vascular stiffness.
- Brain: Worsening neuroinflammation and cognitive decline.
- Lungs: Impairing respiratory function and tissue elasticity.
- Adipose tissue: Driving metabolic dysfunction and insulin resistance.
In other words, wherever they reside, dysfunctional macrophages contribute to the multisystem nature of aging — making them an especially attractive therapeutic target.
A New Discovery: Senescent Macrophages and Their Unique Biology
Recent research has shed light on several distinctive features of senescent macrophages that set them apart from other senescent cells:
- They retain much of their phagocytic (debris-clearing) ability but lose regulatory control over inflammatory signaling.
- They demonstrate increased resistance to apoptosis (programmed cell death), which allows them to persist longer than they should.
- Their metabolic profile shifts toward glycolysis, fueling persistent inflammation.
- They secrete higher levels of damaging cytokines such as IL-6, TNF-alpha, and MCP-1, which recruit more inflammatory cells and worsen tissue dysfunction.
This unique combination of characteristics makes them particularly dangerous during aging — but also uniquely targetable for therapeutic intervention.
Senolytics vs. Senomorphics: How to Tame Senescent Macrophages
Researchers are now exploring two primary strategies to mitigate the harmful effects of senescent macrophages:
1. Senolytic Therapies
Senolytics are compounds designed to selectively induce cell death in senescent cells while sparing healthy ones.
- Early studies using drugs like dasatinib and quercetin have shown promise in clearing senescent macrophages.
- Removing these dysfunctional cells may help reduce systemic inflammation, improve tissue function, and slow disease progression.
However, because macrophages serve critical functions in host defense, senolytic approaches must be carefully balanced to avoid impairing immune responses.
2. Senomorphic Therapies
Senomorphics (or senostatics) aim to modulate the inflammatory behavior of senescent cells rather than eliminating them.
- Drugs targeting NF-kB signaling or mTOR pathways have shown potential to quiet the SASP profile.
- This may allow senescent macrophages to persist while reducing their inflammatory damage.
Senomorphic approaches may offer a safer alternative in situations where wholesale removal of immune cells might create unintended risks.
Why This Discovery Is So Important for Longevity Science
Senescent macrophages sit at the intersection of multiple aging processes:
- Chronic inflammation (inflammaging)
- Immune dysregulation (immunosenescence)
- Tissue fibrosis and scarring
- Metabolic disorders
- Neurodegeneration
By identifying senescent macrophages as a common driver of multisystem aging, researchers may be able to design interventions that provide broad, systemic health benefits, rather than simply treating isolated diseases.
In many ways, senescent macrophages act as keystone contributors to the entire aging process.
Clinical Implications: Where Might These Therapies Help Most?
Targeting senescent macrophages could potentially benefit a wide range of age-related diseases, including:
- Atherosclerosis: Reducing vascular inflammation and plaque buildup.
- Alzheimer’s disease: Quieting microglia-driven neuroinflammation.
- Osteoarthritis: Minimizing joint degradation and cartilage loss.
- Liver fibrosis: Preventing scarring and functional decline in fatty liver disease.
- Type 2 diabetes: Improving insulin sensitivity and metabolic flexibility.
- Pulmonary fibrosis: Preserving lung function in chronic respiratory conditions.
Each of these diseases shares a common inflammatory thread that may be traceable, at least in part, to senescent macrophage dysfunction.
Personalized Medicine: The Future of Targeting Senescence
As the field of senescence biology evolves, we may move toward highly personalized strategies for managing senescent macrophages based on:
- Genetic predispositions
- Tissue-specific senescence profiles
- Inflammatory biomarker signatures
- Metabolic health status
Future clinical testing may include senescence biomarker panels, allowing individuals to track the presence and activity of senescent macrophages — and intervene early, before organ damage accumulates.
What Can We Do Today? Lifestyle Strategies to Support Healthy Macrophage Function
While targeted senescence therapies remain in development, we can take meaningful steps today to preserve healthy macrophage function and minimize chronic inflammation:
1. Anti-Inflammatory Diet
- Polyphenol-rich foods: berries, olive oil, turmeric, green tea.
- Omega-3 fatty acids: wild fish, flaxseed, algae oil.
- Fiber-rich plant foods to support the gut microbiome, which influences immune balance.
2. Regular Physical Activity
- Exercise improves macrophage plasticity, enhancing their ability to switch between pro-inflammatory and repair modes as needed.
3. Intermittent Fasting or Time-Restricted Eating
- These metabolic stressors activate autophagy, improving cellular cleanup and reducing senescent burden.
4. Sleep Optimization
- Deep, restorative sleep promotes immune resilience and proper macrophage function.
5. Stress Reduction
- Chronic psychological stress accelerates immune dysregulation; mindfulness practices and nature exposure can buffer this effect.
The Delicate Balance: Not All Senescence Is Bad
It’s important to remember that senescence evolved as a protective mechanism, especially in immune cells like macrophages. In certain contexts, senescent macrophages:
- Help limit infection spread
- Prevent tumor formation
- Coordinate wound healing
Our challenge is not to eliminate senescence altogether, but rather to modulate its harmful chronic overactivation, restoring the delicate balance between defense and degeneration.
Final Thoughts: The Next Chapter in Precision Longevity
The discovery of senescent macrophages as a unique aging target signals a new level of sophistication in our understanding of longevity:
- No longer is aging seen as one uniform process to slow.
- Instead, it’s a collection of highly specific dysfunctions — many of which may be safely, gently corrected.
As therapies emerge that selectively address senescent macrophages, we may gain a powerful new lever to extend healthy years of life, not simply by treating diseases after they emerge, but by preventing tissue dysfunction before decline sets in.
With each new discovery like this, the horizon of healthy aging grows closer — offering not just longer life, but a life that remains vibrant, strong, and fully lived.
