Multiple sclerosis (MS) has long puzzled researchers. Unlike many chronic illnesses, it does not follow a simple cause-and-effect pattern. Instead, it appears to arise from a tangled interplay of genetics, immune dysfunction, inflammation, environmental factors, and — as scientists are now beginning to understand — a surprising biological phenomenon known as epigenetic memory.
While this research is highly relevant for people living with MS, it may also hold profound implications for how we think about inflammation, immunity, and the broader aging process itself. Let’s explore how this emerging science may shed light not only on MS but also on the ways in which our immune system remembers — and sometimes misremembers — how to function.
What Is Epigenetic Memory?
Before we dive into multiple sclerosis, let’s briefly review this powerful biological concept.
Epigenetic memory refers to how our cells “remember” past experiences not by altering our DNA sequence, but by changing how genes are expressed. This happens through chemical modifications like:
- DNA methylation (adding methyl groups to DNA, turning genes on or off)
- Histone modification (altering how tightly DNA is wound around proteins)
- Chromatin remodeling (changing how accessible genes are for transcription)
These epigenetic tags control which genes are activated or silenced in different situations. They allow your cells to adapt to environmental cues — such as infection, injury, or stress — and maintain these responses even after the original trigger has passed.
In many ways, epigenetic memory is a crucial part of how we stay alive. It helps our immune system learn from past infections and enables wound healing. But in certain situations — like MS — these same mechanisms may go awry, locking the immune system into a damaging, self-sustaining loop of inflammation.
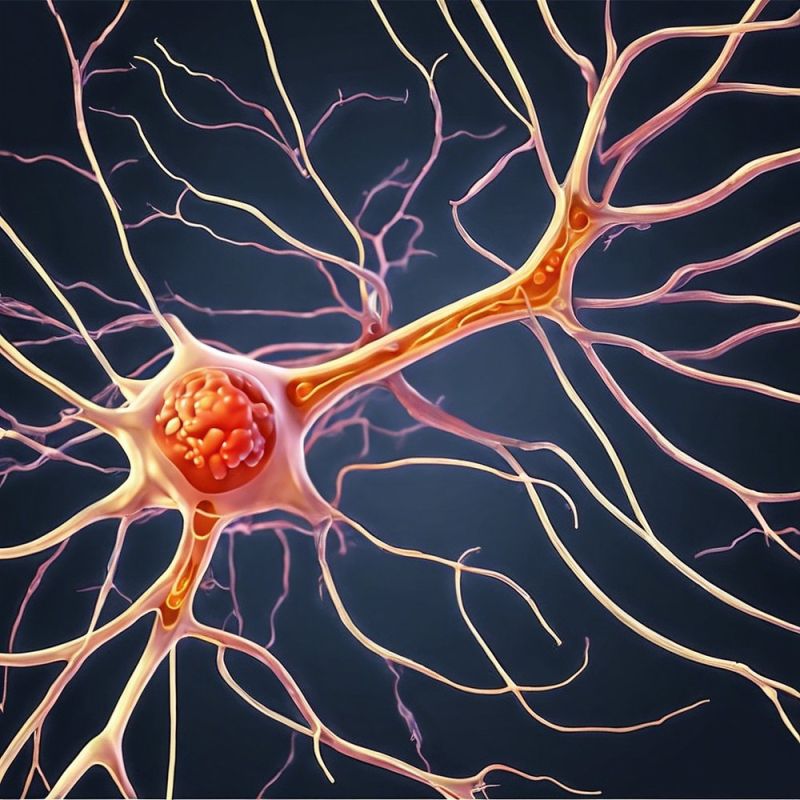
Multiple Sclerosis: A Disease of the Immune System’s Memory?
MS is an autoimmune disorder in which the immune system mistakenly attacks the protective sheath (myelin) surrounding nerves in the brain and spinal cord. This leads to impaired nerve signaling, muscle weakness, balance problems, and often progressive disability.
While many factors contribute to MS — including genetic susceptibility, viral infections, and environmental exposures — researchers have long struggled to explain why the immune system stays chronically overactive long after an initial trigger may have passed.
Now, epigenetic memory offers a compelling new explanation.
The Study: How Epigenetic Memory May Fuel MS
In a recent study published by researchers from the Netherlands, blood cells from people with MS were compared to those from healthy individuals. The scientists focused on CD4+ T cells, a type of immune cell central to orchestrating both defense against pathogens and — unfortunately — autoimmune attacks.
What they found was striking:
- T cells from MS patients showed widespread differences in DNA methylation patterns compared to healthy controls.
- These epigenetic changes were not random — many occurred in genes involved in immune activation, inflammation, and cell survival.
- The altered methylation landscape essentially “primed” the cells to overreact to inflammatory signals, even when no clear external threat was present.
In other words, the immune cells seemed to carry a dysfunctional memory of past inflammatory events — a kind of biological scar that kept them locked in attack mode.
Why This Matters: The Persistence of Inflammatory Memory
The idea that immune cells can hold on to damaging epigenetic memories offers several powerful insights:
- Explains disease persistence: Even if the original trigger for MS is gone, epigenetically reprogrammed cells continue to misfire.
- Explains relapses: Once trained into hyper-reactivity, immune cells may be more easily provoked by minor stimuli.
- Explains progression: Over time, the accumulation of these changes may drive worsening disability, even without active inflammation.
This may also help explain why certain MS treatments — such as immunosuppressants — can reduce symptoms but may not fully reverse disease course: they control active inflammation but may not erase the deeper epigenetic imprinting.
Epigenetic Memory: A Double-Edged Sword in Aging
While this research focused on MS, the concept of harmful epigenetic memory may extend far beyond autoimmune disease. As we age, our bodies accumulate thousands of tiny cellular “memories” of past stress, damage, and inflammation:
- Chronic infections
- Environmental toxins
- Metabolic imbalances
- Poor sleep, stress, or trauma
Over time, these influences may reshape the epigenetic landscape in many tissues, contributing to:
- Persistent low-grade inflammation (sometimes called “inflammaging”)
- Loss of tissue repair capacity
- Increased vulnerability to chronic diseases
In this way, epigenetic memory may serve as a bridge between lifetime exposures and biological aging — not because our DNA changes, but because how that DNA is read and used shifts progressively toward dysfunction.
Is Epigenetic Memory Reversible?
Perhaps the most exciting question is whether these damaging epigenetic patterns can be safely reversed. Encouragingly, the answer may be yes.
Early studies in epigenetic reprogramming — including groundbreaking work in Yamanaka factors (cellular reprogramming genes) — suggest that certain epigenetic marks can be reset, at least partially, restoring cells to a more youthful or functional state.
While wholesale reprogramming carries risks (such as cancer), researchers are exploring partial reprogramming protocols that may selectively erase harmful epigenetic changes without resetting cell identity entirely.
For conditions like MS, this opens the door to potential future therapies that don’t simply suppress the immune system but reset its epigenetic programming back toward healthy function.
Potential Longevity Applications
Even outside of autoimmune diseases, understanding and targeting epigenetic memory may yield novel strategies for extending healthspan:
- Preventing inflammaging by dampening chronic inflammatory gene expression
- Enhancing tissue regeneration by restoring youthful epigenetic programs
- Protecting cognitive function as brain aging may involve cumulative epigenetic dysfunction
- Improving metabolic flexibility through reprogramming genes involved in insulin sensitivity and lipid metabolism
While this field remains young, epigenetic interventions could ultimately form a cornerstone of personalized anti-aging medicine.
How Lifestyle May Influence Epigenetic Memory
While cutting-edge therapies are still in development, several everyday choices may help prevent harmful epigenetic memory formation or even promote healthier gene expression:
1. Anti-inflammatory Diet
- Emphasize plant-rich, polyphenol-heavy foods (berries, greens, turmeric, olive oil)
- Limit processed foods and added sugars that drive oxidative stress
2. Regular Exercise
- Physical activity has been shown to modify DNA methylation patterns linked to inflammation and aging
3. Stress Management
- Chronic stress reshapes epigenetic patterns in immune and brain cells; mindfulness, meditation, and breathwork may counteract this
4. Quality Sleep
- Sleep regulates circadian gene expression, which in turn influences epigenetic stability
5. Avoid Environmental Toxins
- Smoking, pollution, and chemical exposures directly damage DNA and modify epigenetic marks
These lifestyle factors likely work not by altering your genetic code, but by shaping how your genes are expressed over time — the very essence of epigenetic memory.
The Road Ahead: Hope Through Precision
Epigenetic memory research is still in its infancy, but it offers an elegant framework that could unify many threads of aging, chronic disease, and immune dysfunction.
For MS, this work raises the possibility that future therapies could focus not only on controlling inflammation but on retraining the immune system’s epigenetic blueprint.
For the rest of us, it suggests that aging need not be a passive process of accumulating damage, but rather an adaptive dance between our environment, our biology, and the choices we make daily.
Final Reflections
The story of epigenetic memory is a powerful reminder that our bodies are not static. We carry with us the imprints of our history — but those imprints may also be flexible, even erasable.
As research advances, we may one day learn to edit our biological memory in ways that preserve the wisdom of experience while shedding the scars of dysfunction. In doing so, we could not only better treat diseases like multiple sclerosis but reshape how we approach health, resilience, and longevity itself.The science is complex, but the message is simple:
How we live today echoes in our cells tomorrow — sometimes for better, sometimes for worse — but increasingly, with hope for renewal.
